A two-year comparative study of admissions of term neonates for hypoglycaemia: what have the BAPM recommendations changed?
Hypoglycaemia is a leading cause of term admissions to neonatal units but many term babies admitted for hypoglycaemia could be cared for in an alternative hospital or community setting. The British Association of Perinatal Medicine (BAPM) Framework for Practice aims to reduce national variation in detection and management of term babies with hypoglycaemia. The study presented here compares the epidemiology of neonatal hypoglycaemia in term neonates admitted to a tertiary neonatal intensive care unit for a one-year period before and after implementation of a BAPM recommendations-based guideline.
Praveen Kishore
MRCPCH
Specialty Registrar (Neonatology)
praveen.kishore@porthosp.nhs.uk
Rahul Kachroo
MBBS, MD, MRCPCH
Consultant Neonatologist
Queen Alexandra Hospital Neonatal Unit,
Portsmouth Hospitals NHS Trust
Background
As part of the Atain programme (Avoiding term admissions into neonatal units), NHS Improvement prioritised the reduction of admission of full term infants (>37 weeks’ gestation) to neonatal units because admission to neonatal care can indicate harm and results in the separation of mother and baby.1
The Atain work focused on four key areas − hypoglycaemia, jaundice, respiratory conditions and asphyxia − and sought to understand the contributory factors leading to these admissions. Hypoglycaemia is a leading cause of term admission to a neonatal unit and many term babies admitted for hypoglycaemia do not receive any intervention that could not have been provided in a hospital or community setting that kept the mother and baby together.1
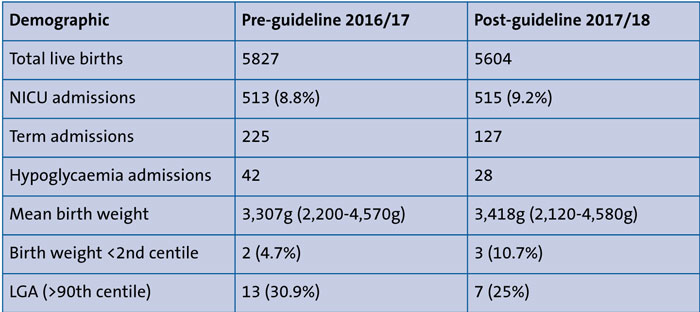
TABLE 1 The demographic characteristics of the pre- and post-guideline periods.
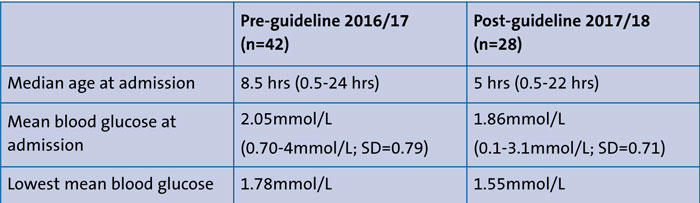
TABLE 2 Term infants admitted to the NICU: age at admission and glucose levels.
In April 2017 BAPM proposed new recommendations for identification and management of hypoglycaemia.2 The BAPM Framework for Practice aims to address variation in practices in the identification, management and admission thresholds of babies admitted to neonatal units for hypoglycaemia. The recommendations include:
- a change in blood glucose threshold for intervention and diagnosis
- exclusion of large for gestational age (LGA) babies from routine screening
- an algorithm for close monitoring while avoiding admission of asymptomatic hypoglycaemia to the neonatal intensive care unit (NICU) for newborn infants born at term.
The neonatal unit at Queen Alexandra Hospital (QAH), Portsmouth, is a tertiary NICU offering medical intensive, high and special care to preterm and sick term babies born in and around Portsmouth, the Wessex region and further afield. Based on the BAPM recommendations, the neonatal unit implemented a new local guideline from 1st July 2017 for management of neonatal hypoglycaemia in term neonates (FIGURE 1).
The study presented here compares the epidemiology of neonatal hypoglycaemia in term neonates admitted to the tertiary NICU for a one-year period before and after the implementation of the BAPM recommendations-based guideline.
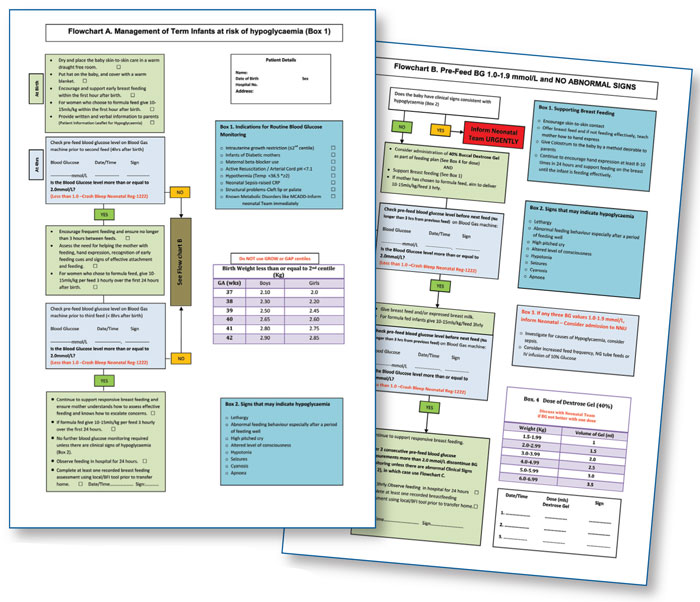
FIGURE 1 The QAH guideline for management of neonatal hypoglycaemia.
Methods
This was a retrospective comparative study analysing case notes and Badger Neonatal Clinical Information System (BadgerNet) summaries. Two different time periods were compared:
- pre-guidelines 1st July 2016 to 30th June 2017
- post-implementation of management guidelines for hypoglycaemia based upon BAPM recommendations, 1st July 2017 to 30th June 2018.
Results
TABLE 1 shows the demographic characteristics of the pre- and post-guideline periods. There were 42 hypoglycaemia term admissions out of 5,827 total live births in the pre-guideline 2016/17 period compared with 28 out of 5,604 in the post-guideline 2017/18 period. This represents a considerable decline in admissions – from 7.2 per 1,000 live births to 4.99 following implementation of the recommendations.
LGA babies continue to be an important group of term infants admitted for neonatal hypoglycaemia (25% post-guideline versus 30.9% pre-guideline). This raises the question of whether LGA should be made an independent criterion for screening again.
TABLE 2 shows the age of admitted term infants, their mean blood glucose level at admission and lowest mean blood glucose level. The cut off following implement-ation of the new guidelines for term infants is 2.0mmol/L. Blood glucose levels were lower for the post-guideline period, perhaps indicating that only infants with a more severe form of neonatal hypo-glycaemia were admitted to the NICU.
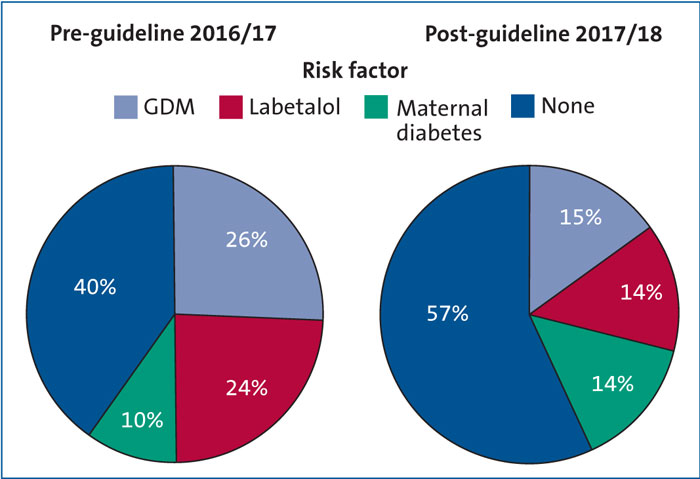
FIGURE 2 Maternal risk factors for hypoglycaemia.
Key: GDM = gestational diabetes mellitus.
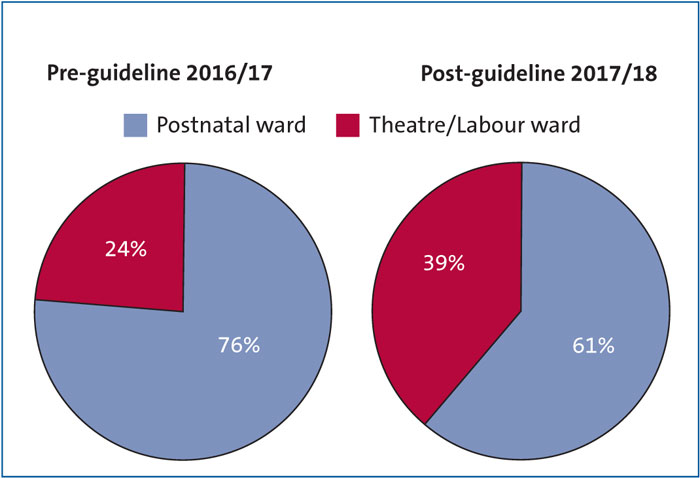
FIGURE 3 Admission sources.
FIGURE 2 shows any maternal risk factors for neonatal hypoglycaemia. Note that labetalol is a beta-blocker used to treat pregnancy-induced hypertension and has been implicated in the aetiology of neonatal hypoglycaemia.3 FIGURE 3 shows the source of infant admissions. Interestingly, fewer babies in 2017/18 (60.7%) were admitted from the postnatal ward compared with 2016/17 (76.2%).
The form of treatment given can be seen in FIGURE 4. In the pre-guideline period, 26.2% of infants improved with feeding support only. Following implementation of the guideline, 7.1% of newborns required feeding support only. Significantly more babies (p=0.044) in the post-guideline population (92% vs 73.8%) needed intravenous dextrose treatment, as compared to feeding support only. Up to 21.4% needed dextrose at 20% concentration. In conjunction with the glucose levels data in TABLE 2, it might be concluded that the less severe forms of neonatal hypoglycaemia – those not needing admission to the NICU – were managed on the postnatal ward in the post-guideline period.
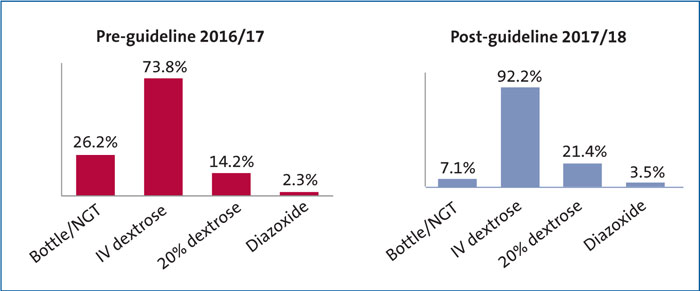
FIGURE 4 The type of treatment given for neonatal hypoglycaemia in term neonates admitted to the NICU. Key: NGT = nasogastric tube feeding.
Conclusion
Hypoglycaemia can lead to significant morbidity and mortality if not recognised and treated promptly but admission to the NICU results in the separation of mother and baby and should be avoided where possible. A local guideline introduced at QAH successfully reduced admissions by identifying only those infants needing IV fluids and further treatment. Term infants with less severe hypoglycaemia can be managed with feeding support on the postnatal wards.
Or read this article in our
Tablet/iPad edition
- The BAPM Framework for Practice addresses identification, management and admission thresholds of babies admitted to neonatal units for hypoglycaemia.
- A local guideline has helped to reduce term admissions for neonatal hypoglycaemia.
- Admitted babies are more likely to need intensive care and less likely to improve with nutritional support alone.
Also published in Infant: