The impact of a local QI project to avoid hypothermia and maintain normothermia in preterm infants following delivery
Maintaining normothermia reduces morbidity and mortality of preterm infants. The aim of this quality improvement (QI) project was to improve compliance with the National Neonatal Audit Programme (NNAP) standard of >90% of infants born at <32 weeks’ gestation having an admission temperature of 36.5-37.5°C. The project assesses outcomes in a tertiary medical neonatal intensive care unit before and after introducing a set of improvement measures, and reports the long-term sustainability since the initial project completed.
Ceri Murphy
Neonatal Grid Trainee
Laura Kelly
Beya Obe Bonse
Rachel Job-Vinu
Silvy Koshy
Mina Wanti
Practice Development Nurses
Claire Howarth
Neonatal Consultant
claire.howarth@nhs.net
Background
Maintaining a normal thermal environment is a key challenge faced by newborn infants immediately after delivery and it is essential for survival. Hypothermia increases the risks of morbidity and mortality significantly.1,2 The International Liaison Committee on Resuscitation (ILCOR) published guidance based on a consensus statement that all newborn infants should have their temperature maintained between 36.5°C and 37.5°C after birth, through stabilisation and on admission.1,2
Given the recent British Association of Perinatal Medicine (BAPM) guidelines on the management of extreme preterm infants where we now may consider offering resuscitation at 22 weeks’ gestation;3,4 optimising admission temperatures for these preterm infants at the edge of viability who are even more vulnerable to hypothermia, is more vital than ever.
Rates of ‘in-range’ admission temperatures for preterm infants born at <32 weeks’ gestation have been consistently low at Homerton University Hospital Neonatal Intensive Care Unit (NICU) and well below the national average. The NICU is a tertiary level medical unit providing intensive care to infants from 22 weeks’ gestation and admits approximately 150 preterm infants <32 weeks’ gestation per year. It is part of the North Central and East London Neonatal (NCEL) network which consists of 11 neonatal units including special care baby units (SCBU), local neonatal units (LNU) and NICUs.
Since 2015, one of the National Neonatal Audit Programme (NNAP) audit measures has been ‘Does an admitted baby born at less than 32 weeks gestational age have a first measured temperature of 36.5°C to 37.5°C within one hour of birth?’ The NNAP sets a standard that the composite measure of timeliness and normal temperature should be met for at least 90% of babies. Since being highlighted as an audit measure, a gradual improvement in the national average was seen each year (57.5% in 2015; 60.5% in 2016; 64.4% in 2017; 67.4% in 2018; 69.9% in 2019, and 70.6% in 2020).5 Despite this, no neonatal unit has consistently achieved the developmental standard of 90%, perhaps highlighting this as a national issue.
There are many QI studies published in the literature reporting improvements in normothermia across multiple settings and countries. Various methods to maintain normothermia and prevent heat loss have been used including the use of plastic bags or wraps, continuous temperature monitoring, monitoring of temperature during stabilisation, allocation of a specific person to monitor thermoregulation during stabilisation, use of transwarmers and targeted education and training.5-13 However, the available evidence suggests that using several methods of heat loss simultaneously is more effective than one intervention alone.14-16 This is why we chose to create a ‘bundle’ incorporating many methods simultaneously.
Aim
Our initial aim was to improve the percentage of infants with an in-range admission temperature to >70% within six months. Because our in-range was so far below the NNAP standard we agreed to start with this target as the first realistic goal and then to subsequently strive to achieve the NNAP standard of at least 90% compliance.
Methods
We conducted a retrospective audit of all infants born at <32 weeks’ gestation admitted to Homerton University Hospital NICU over one year (1 August 2018 to 1 August 2019) and showed that only 55% had a normal admission temperature of 36.5-37.5°C (n=87; birth weight=440-2,075g; gestational age=23+0 to 31+6 weeks). 37% had an admission temperature <36.5°C and 8% had an admission temperature >37.5°C. This information was taken from the BadgerNet database, which collects data for the NNAP.
According to the latest NNAP data at the time we started the project, we were below the national average of 67.4% and well below the NNAP standard target of >90%. Furthermore, we had remained consistently below target for the past five years, despite the team being more aware of the importance of normothermia and the theoretical ways to avoid hypothermia (52.8% in 2015; 51.7% in 2016; 54.6% in 2017, 60.8% in 2018 and 56.8% in 2019).5 In addition, our NCEL network compliance was well below target (51.8% in 2015; 52.2% in 2016; 61.6% in 2017; 62.5% in 2018, and 59.9% in 2019).5
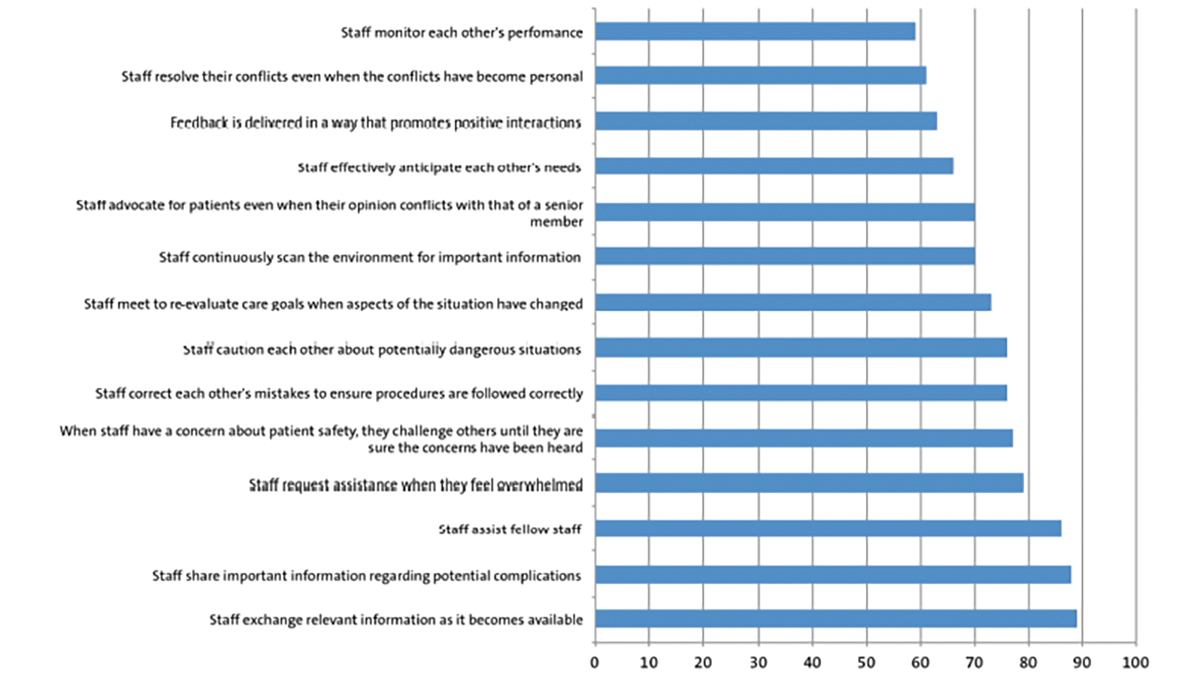
The driver diagram (FIGURE 1) illustrates the risk factors for hypothermia that we identified and aimed to influence. It was important for us to identify risk factors that were applicable for our local practice and introduce these measures to ensure they happened consistently, regardless of the delivery condition of the baby and setting. To implement these, a QI team consisting of a consultant, junior doctors, and practice development nurses (PDN) was formed.
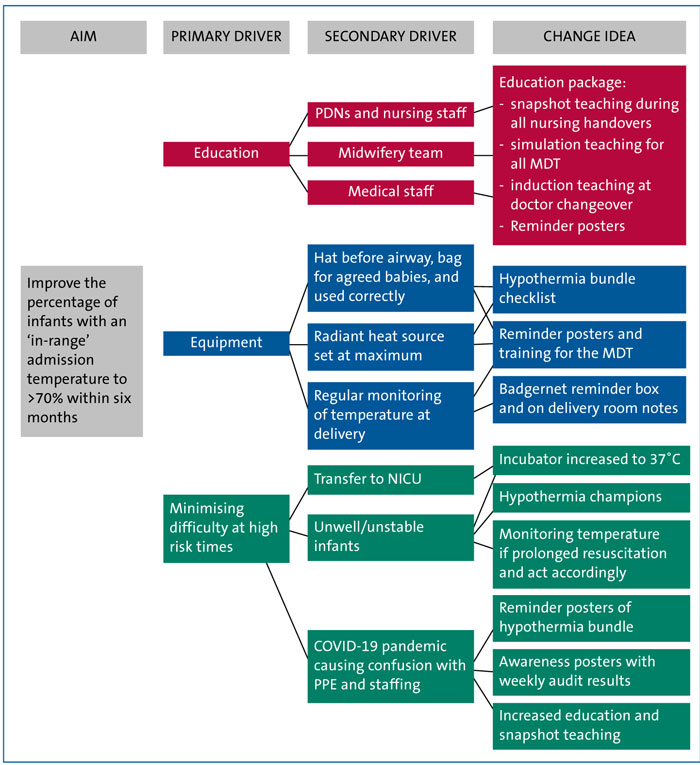
FIGURE 1 Driver diagram.
A teaching session on hypothermia was held and we created a hypothermia prevention bundle (FIGURE 2) using input from the multidisciplinary team (MDT). Daily ‘snapshot’ teaching at each nursing handover was led by PDNs over a two-week period and a poster was displayed in the NICU, labour ward and staff rooms to increase awareness. We found that most people were amenable to change, however we appreciated that we may face difficulties with infants at particularly high risk for hypothermia (for example those requiring prolonged resuscitation and unexpected deliveries where heat loss prevention measures were not available).
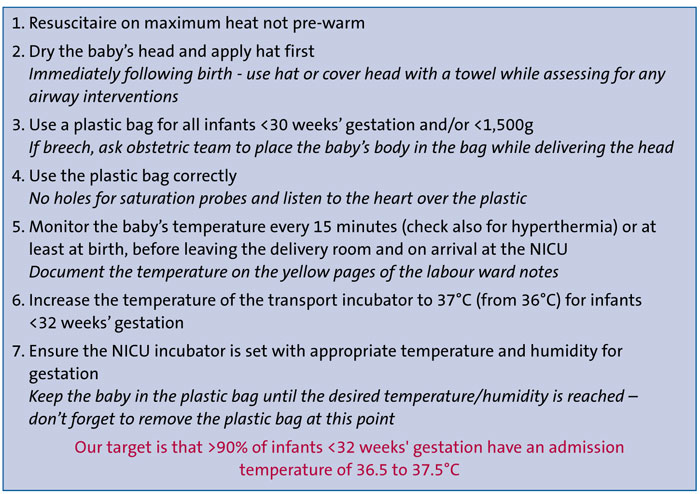
FIGURE 2 The initial Homerton NICU hypothermia prevention bundle, 2019 (this was updated in 2021 in line with the changes to the Newborn Life Support guidelines so that a plastic bag was used for all infants born <32 weeks' gestation, rather than 30 weeks', and/or 1500g).
Results
58 infants were included in the initial QI project from October 2019 to May 2020 (median gestational age=27 weeks; median birthweight=900g).
Overall, during this QI project we achieved a compliance rate of 83% of infants <32 weeks’ gestation having an admission temperature of 35.5-37.5°C (n=48), which was a significant change (p<0.05). For two months, we reached 100% and we therefore achieved our initial aim of improving to >70% admission temperatures in-range. At the end of this QI project, our 2020 average reported by NNAP was 73.8%, which was above our NCEL network average (67.6%) and the national average (70.6%).
Ten infants had admission temperatures out of range: two infants >37.5°C (both due to maternal sepsis) and there were eight infants with an admission temperature <36.5°C (birth weight=452-1,860g; gestational age=22+6-31+4 weeks), although none were <36°C. Of the infants who were admitted hypothermic, they either were very unwell (<29 weeks’ gestation or severe hydrops), needing a lot of resuscitation, born unexpectedly not on labour ward with reduced time for preparation, or the thermal control measures were poorly documented meaning it was unclear if the hypothermia prevention bundle was followed. The average drop in temperature from labour ward to admission temperature was 0.3°C.
Bundle compliance showed that plastic bag use was most consistent for eligible infants; 87% were placed in a plastic bag appropriately; 13% lacked documentation. Just 69% had a hat applied, with 3% not having a hat applied and 28% not documented.
59% had an overhead heater set to maximum heat; 3% did not and 38% lacked documentation. 31% of infants did not have a temperature documented prior to leaving the delivery room; of these, 33% had a temperature out of range.
PDSA cycles
During the initial project we used the ‘plan do study act’ (PDSA) methodology and undertook three PDSA test cycles (FIGURE 3).
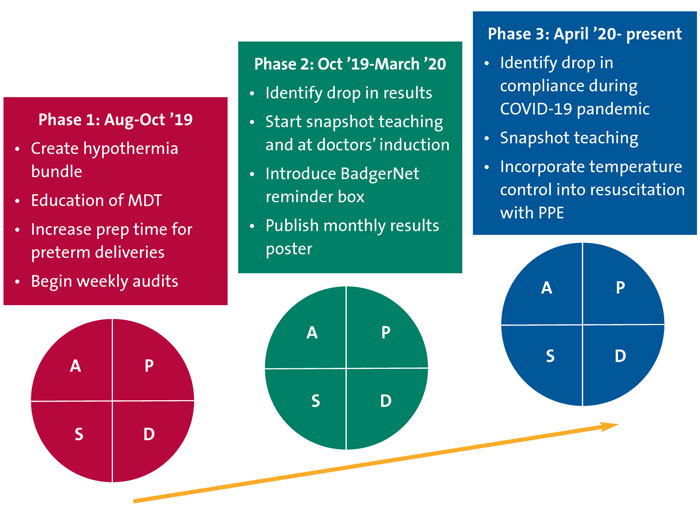
FIGURE 3 The three ‘plan do study act’ (PDSA) cycles.
Cycle 1: August-October 2019
Our aim was to identify and agree on factors that prevent heat loss immediately after delivery to create the hypothermia prevention bundle (FIGURE 2), which would become embedded in standard practice.
Our strategy was to involve the whole MDT via teaching sessions run by doctors and PDNs, testing staff knowledge of the bundle, running simulations of practice and displaying regular reminder posters on the NICU and labour ward. The importance of documenting each heat-loss prevention method was stressed to the whole team. The delivery of a preterm infant is unpredictable with a plethora of situations that could draw attention away from thermal control. We felt that if documentation of this became compulsory, it was more likely to be carried out. The bundle was introduced on 30 September 2019 and by October 2019 the percentage of <32 weeks’ gestation infants with an in-range temperature improved to 89%, compared to 55% before we started.
Cycle 2: October 2019-March 2020
To quickly identify our progress, we conducted weekly audits from October. We saw that there was great enthusiasm for change among our staff in the first month and our admission temperatures improved from 55% in-range to 89% by the end of October. We noted that of those out of range, the infants were more likely to have required more interventions after birth (eg multiple intubation attempts) and documentation in these cases was lacking. We added a reminder box onto the BadgerNet summary requesting temperature to be checked prior to leaving the labour ward during this cycle, which led to an increase in this being documented and an improvement in percentage of admission temperatures in-range to 75-100% (average=87.7% during this cycle). By having the temperature on labour ward documented and then the admission temperature, we could compare the values to see whether temperatures were dropping on route from the labour ward to the NICU.
Cycle 3: April 2020-current
A drop in compliance was seen in April 2020 (67%), which was identified quickly due to our weekly audits. This coincided with the start of the COVID-19 pandemic and during this time, the team was adapting to multiple new guidelines (eg learning to use personal protective equipment, PPE, and staff shortages). We introduced further teaching, including simulations, with our aim being to help the team to integrate PPE and thermal control into standard practice. By using monthly reminder posters displaying results, identifying hypothermia prevention champions and working with midwives to ensure we had adequate time to prepare prior to deliveries (especially those where PPE was needed), we saw a great improvement in our admission temperatures, with 100% in-range the following month. This highlights the importance of the PDSA cycles and regular audits to ensure that compliance is maintained.
Ongoing cycles: post-initial QI project
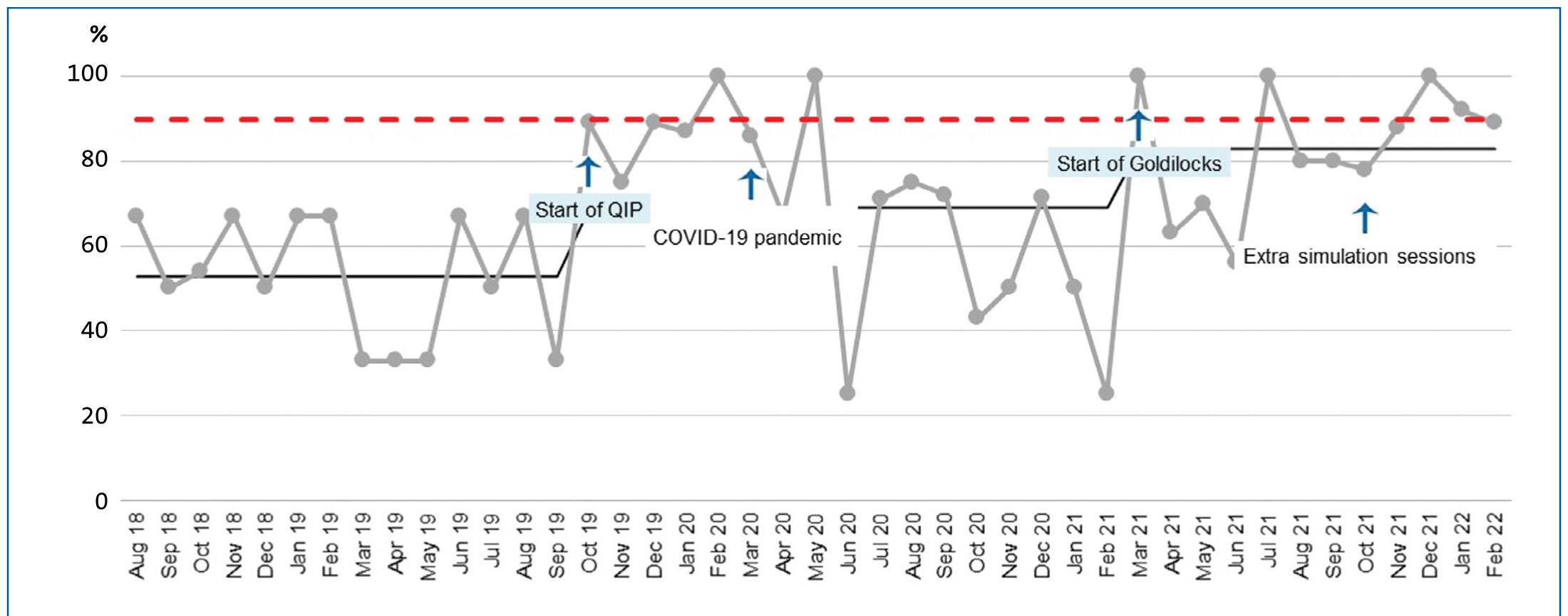
After the initial QI project finished in May 2020, we maintained the collection of monthly data and we implemented further strategies when there were drops in compliance (continuing with the PDSA cycles). Our monthly results to February 2022 are shown in FIGURE 4. We had several months where 100% of infants born at <32 weeks’ had an admission temperature in-range and several where we achieved the 90% NNAP standard. Our mean percentage compliance over the last six months (September 2021 to February 2022) was 87.8%.
Figure 4 Run chart for monthly in-range admission temperatures, including the start of the QI project and the start of the Goldilocks project. The red dashed line represents the NNAP standard of at least 90%. Key: QIP=QI project.
FIGURE 4 shows that after the initial QI project ended, there were drops in compliance in February 2021 and June 2021. In February 2021 the drop in compliance was because there were infants admitted who were hyperthermic (an admission temperature >37.5°C) and therefore we introduced the Goldilocks project in March 2021 to ensure we placed as much focus on avoiding hyperthermia as well as hypothermia. This consisted of further teaching sessions and reiterating the importance of monitoring temperature on the labour ward. In June 2021 the ongoing impact of the COVID-19 pandemic took its toll on our staff and resources. We were able to see improvements just by continuing our monthly reminders, providing teaching at handovers for nursing staff and running more simulation sessions for the whole team.
With the changes to the Newborn Life Support (NLS) guidelines published in May 2021,17 we amended our hypothermia prevention bundle so that a plastic bag was recommended for all infants born <32 weeks’ gestation, rather than 30 weeks’.
Discussion and lessons learned
Our results improved immediately after the hypothermia prevention bundle was implemented, which is commonplace in QI projects when enthusiasm for change is high. One of the main difficulties is sustainability and we learned that by using the weekly and then overall monthly audits, we could quickly see the trends in our target percentage and feed this back to the team in a timely manner while also praising good compliance. Whenever we saw a drop in compliance, we tried to look at why this had occurred, highlighted this to the team and introduced a new cycle (such as extra teaching or adding documentation to the BadgerNet summary). Because everyone must complete the BadgerNet admission summary, it promp-ted them to remember to document the temperature prior to leaving the labour ward. Keeping up awareness of the project and education of the whole team was key to its success, reduced barriers to implementation and now underpins its sustainability.
We learned that any new change needs to be built into existing systems and, until it is fully embedded, regular audits and education must continue to ensure rates of compliance remain high. One inevitable area of reduced compliance is anticipated at our doctor changeovers in September and March of each year, therefore in the September 2020 induction we added a focused talk on this project to ensure all new doctors were aware of it from the outset. This talk is now included in each of our inductions, as well as a simulation session on the use of the plastic bag and hypothermia prevention bundle.
One limitation of all QI projects is achieving sustainable results and we have been able to continue improving by introducing hypothermia prevention champions to each delivery team – a person who will focus on thermoregulation at deliveries and during stabilisation. Also, there is a group of medical and nursing champions who monitor the results and publish these, as well as implement new teaching and simulation if required.
We recorded bundle compliance throughout this QI project to identify all issues relating to sustainability. For the infants admitted hypothermic, the documentation for heat reducing measures was more likely to be low (between 13-38% of measures not documented) and it was also clear that for unexpected deliveries, where the neonatal team had less time to prepare, thermal control was less optimal. Preterm deliveries can and will continue to happen unexpectedly and this is the next focus for the QI project – we are going to explore the use of additional thermal measures, such as transwarmers for babies born unexpectedly where there is insufficient time to prepare an optimum thermal environment.
Success of the same QI measures can vary between settings; there are some neonatal units who achieve excellent compliance with the NNAP admission temperature standard and don’t use occlusive wraps, plastic bags or transwarmers. What was vital in the success of our project was specifically looking at our unit and processes and why our infants were not achieving normothermia on admission. It was only then, that we could decide which interventions would work best for us. We would encourage all units to start with this process first and critically evaluate why their infants are not achieving normothermia before starting any improvement measures.
Staff members reported they felt that using heat maintaining measures enhanced resuscitation and only minimal changes needed to occur (none of which were time consuming), for example placing the saturation probe over the plastic bag instead of exposing the arm outside of the bag. Some infants had a short delay in transfer from the delivery room to the NICU due to low temperature while the team optimised thermal care and waited for normothermia to be achieved. This decision was made by the attending clinician and only for those infants who were stable and already receiving the care they required (eg already on respiratory support). This did not apply to unstable infants who required immediate transfer to the NICU. Clinicians were encouraged to record any delay in the medical notes.
Recent data suggest an association between admission hyperthermia (>38°C) and adverse outcome.18 Within the initial QI project only two of the 58 infants (3.4%) had admission temperatures >37.5°C. While our initial focus was primarily on preventing hypothermia, since March 2021 we have been focusing as much attention on preventing hyperthermia with the new Goldilocks campaign: ‘not too hot, not too cold, just right’.
Prior to this project, we had made very little progress in improving admission temperatures and in recent years we were persistently below the network and national average. This was possibly due to a lack of awareness by the whole MDT with a focus on other measures, such as quality of resuscitation. One strategy we also used after the initial QI project finished was to have core individuals going to preterm deliveries and observing what was happening in terms of the use of the hypothermia prevention bundle. This was imperative as it allowed us to see any issues and then educate the team. By involving the nursing staff and inspiring the whole MDT to be responsible, we have seen an excellent response. For a QI project, it is not unusual for the level of improvement to reduce over time; however, we have sustained our improvement because we continue with the monthly audits and our hypothermia prevention champions.
Conclusion
We surpassed our aim of increasing in-range admission temperatures to above 70% within six months. The project is still ongoing to ensure sustainability of this improvement, with regular audits and our hypothermia prevention champions. We have embedded the hypothermia prevention bundle into our routine practice and the monthly results are discussed in our neonatal governance meetings and at network meetings. Our goal is to ensure that we continue to achieve the NNAP standard of at least 90% of infants born at <32 weeks' gestation having an in-range admission temperature.
Author contribution statement and acknowledgements
CH conceptualised the QI project, carried out the initial audit, designed the hypothermia prevention bundle and co-led the education for the medical team. CM collected, analysed and published the monthly results and co-led the education of the medical team, including the posters, teaching presentations and postgraduate presentations. CM wrote the first draft of the article. The PDNs, LK, BB, RJV, SK and MW, were responsible for agreeing the initial hypothermia prevention bundle, educating the nursing staff, and giving regular reminders at nursing handover. All authors reviewed and revised the manuscript.
The authors would like to thank all the PDNs who worked so hard at educating the large nursing team, and their medical and nursing colleagues who continue to work hard to improve preterm admission temperatures.
Or read this article in our
Tablet/iPad edition
- Simple measures are effective at ensuring normothermia, but units must specifically examine why they are not meeting targets before implementing improvement measures.
- Keeping up awareness and educating the whole team is key to success. Having motivated champions to maintain momentum and feeding back results quickly enables sustainability.