Syphilis: a re-emerging infection with potentially fatal consequences for the neonate
This report discusses a case of a sick newborn who was diagnosed with congenital syphilis. With rising rates of syphilis infection and opportunities for missed antenatal diagnosis, this report aims to remind clinicians of the importance of early diagnosis and treatment of congenital syphilis to prevent serious complications and mortality for the neonate.
Tochi Igboekw
Paediatric ST8
Khalida Yasso
Paediatric ST5
kyasso@nhs.net
Emily Thomas
Paediatric ST8
Emily Rye
Paediatric ST1
Sally Ogden
Neonatal Consultant
Neonatal Unit, Whiston Hospital, St Helen’s and Knowsley NHS Trust Neonatal Unit, Liverpool Women’s Hospital, Liverpool Women’s NHS Foundation Trust
Background
There is a recent national resurgence of syphilis infection rates.1 Public Health England data report rising rates of syphilis cases in the adult population with an increase of 162% between 2008 and 2018.1
As rates of syphilis rise in the general population, neonatologists and paediatricians should be aware that, consequentially, congenital syphilis cases may increase. A 2018 annual European epidemiological report found that rates of congenital syphilis were on the rise for the first time since 2013.2 Opportunities for missed antenatal diagnosis may arise in patients born to mothers who are negative for syphilis at booking or who have not received the usual antenatal care.
It is estimated that up to 40% of babies with congenital syphilis may be stillborn or die as a newborn.3 Infected infants may experience severe sequelae, including cerebral palsy, hydrocephalus, sensori-neural hearing loss and musculoskeletal deformity.4
The challenge clinicians face is the variable presentation of congenital syphilis as well as the fact it can mimic more common differentials, earning itself a reputation as the ‘great imitator’.5 This can result in a delay in diagnosis and treatment, increasing the risk of severe disability to the neonate.
We report a case of a late preterm male infant who presented critically unwell within hours of birth, the cause of which was later attributed to congenital syphilis. We hope this case and subsequent discussion will serve as an aide memoire to clinicians to consider congenital syphilis as a potential diagnosis, even with a seemingly uncomplicated antenatal course.
The case
Baby S was born at 35 weeks’ gestation by category two caesarean section with forceps assist, due to reduced fetal movements and pathological cardiotocography. This was on a background of spontaneous premature labour and possible spontaneous premature rupture of membranes three days prior to delivery.
There had been a history of a small antepartum haemorrhage at 25 weeks’ gestation. Beyond this, the antenatal history was unremarkable with normal blood tests at booking (including a negative syphilis, HIV and hepatitis B screen) and no concerns raised on routine antenatal scans or appointments.
Baby S was born with no respiratory effort and poor tone but responded well to stimulation with Apgar scores of 7, 8 and 9 at one, five and 10 minutes. His birth weight was 2.48kg on the 50th centile and head circumference on the 75th centile. Intermittent grunting and reduced tone were noted at 10 minutes of life. He appeared increasingly pale despite normal oxygen saturation levels in air. He was transferred to the neonatal unit for a septic screen and further observation.
On arrival at the special care baby unit (within one hour of age), Baby S was haemodynamically stable (respiratory rate=55 breaths per minute; oxygen saturation=98% in room air; heart rate=161 beats per minute; blood pressure=63mmHg/30mmHg; mean arterial blood pressure=40mmHg; temperature=36.4°C) but was noted to be clinically jaundiced and anaemic. Cord blood tests and first venous gas analysis showed a picture of metabolic acidosis with anaemia and hypoglycaemia.
At this stage, the differential diagnoses were:
- sepsis resulting in hypoglycaemia and anaemia
- haemolytic anaemia
- acute blood loss.
Baby S was commenced on intravenous antibiotics within one hour of age (IV benzylpenicillin and IV gentamicin, in keeping with trust policy). His hypoglycaemia was corrected. Blood tests were sent for full blood count, C-reactive protein (CRP), blood culture, serum bilirubin, blood group and direct antibody test and crossmatch.
Unfortunately, he continued to deteriorate and at two hours of life a repeat capillary gas test showed worsening metabolic acidosis, profound hypoglycaemia of 0.5mmol/L and lactate rising to 6.2mmol/L (TABLE 1).
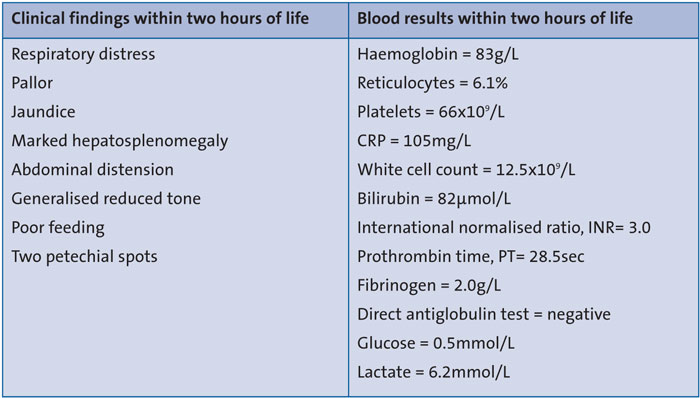
TABLE 1 Key findings within two hours of life.
At this time, the clinical examination revealed mild respiratory distress, jaundice, pallor, generalised reduced tone and a distended abdomen with palpable hepato-splenomegaly (TABLE 1). When the blood tests returned, they demonstrated jaundice near the exchange transfusion level, anaemia, thrombocytopenia, raised inflammatory markers and a picture of disseminated intravascular coagulation.
The infant was treated with glucose and fluid boluses, a packed red cell transfusion, and half bicarbonate correction as well as repeat vitamin K and fresh frozen plasma, following discussion with the on-call haematologist.
Further investigations were sent to enable a metabolic screen. A repeat maternal TORCH screen was requested. Chest and abdominal X-rays and cranial ultrasound were performed to exclude active bleeding.
Despite the management steps, repeated blood gas tests showed worsening metabolic acidosis and Baby S developed an increasing oxygen requirement. He was commenced on high flow oxygen therapy due to respiratory distress.
Given the worsening clinical picture, the team decided to electively intubate Baby S and transfer him to a tertiary neonatal unit. Umbilical arterial and venous access was achieved after initial attempts had been abandoned due to excessive bleeding. Following intubation, he became hypotensive and developed an increasing oxygen requirement.
He stayed in this tertiary centre for 16 days, requiring intensive care for six days with ventilation, inotropic support and fluid resuscitation with repeated blood products and clotting factors. Following this, he was stepped down to high dependency care. During this time, he was noted to have deranged liver enzymes and clotting factors as shown in TABLE 2.
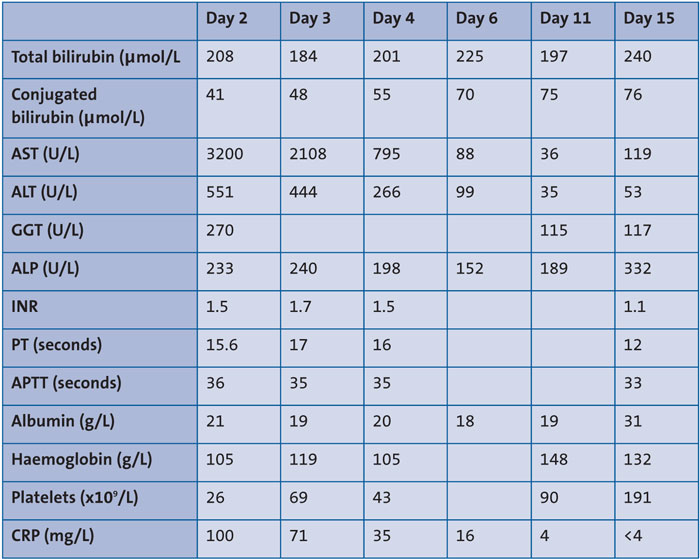
TABLE 2 Liver function tests while in the tertiary centre. Key: AST = aspartate aminotransferase, ALT = alanine aminotransferase, GGT = gamma-glutamyl transferase, ALP = alkaline phosphatase, INR = international normalised ratio, PT = prothrombin time, APTT = activated partial thromboplastin time, CRP = C-reactive protein.
Further investigations were undertaken to identify a diagnosis for his liver dysfunction alongside advice from the specialist liver unit. Abdominal ultrasound showed diffuse liver hypoechogenicity consistent with neonatal hepatitis and ascites. A repeat ultrasound scan on day 13 showed the liver parenchyma had returned to normal with minimal ascites and a normal biliary tract.
The repeat maternal TORCH screen taken on the day of delivery confirmed syphilis infection with an RPR (rapid plasma regain) ratio of 1:32 and TPPA (Treponema pallidum particle agglutination assay) of 1:>5,120 consistent with a recent untreated infection. Paired syphilis serology was taken on Baby S and his mother on day 13 of life and the results were:
- RPR ratio: Baby S = 1:1; mother = 1:256
- TPPA ratio: Baby S = 1:256; mother = 1:5,120
- IgM antibody: Baby S = positive; mother = positive
The infant was initially treated with a seven-day course of IV benzylpenicillin for suspected sepsis prior to the diagnosis of congenital syphilis. His blood culture and cerebrospinal fluid (CSF) culture were negative. Following discontinuation of the antibiotics it was noted that his transaminases, which had normalised, were starting to worsen again. The diagnosis of congenital syphilis came on day 13 and after discussion with the infectious disease specialists, a full 10-day treatment of high dose IV benzylpenicillin (50mg/kg, three times a day) was restarted due to concerns that the previous course may have only partially treated the infection. Further serology was sent for other blood-borne infections, including HIV and hepatitis B/C, which were all negative. A lumbar puncture was performed but unfortunately the CSF obtained was insufficient for further VDRL testing (venereal disease research laboratory test; syphilis) or RPR, although the cell count was normal.
X-rays of the long bones, cranial ultrasound and an ophthalmology review were all unremarkable for complications of syphilis. Histology from the placenta was also consistent with congenital syphilis infection and necrotising granulomatous villitis was seen.
The infant was discharged at day 24 of life and remains well in the community with close monitoring of growth and potential complications.
Discussion
Congenital syphilis occurs when maternal infection with Treponema pallidum spirochetes is transmitted via the trans-placental route to the fetus. In untreated maternal cases there is near 100% transmission. Most cases worldwide occur due to lack of prenatal care or insufficient treatment during pregnancy and globally congenital syphilis remains a prevalent and concerning cause of perinatal morbidity and mortality. A meta-analysis published by the World Health Organization (WHO) in 2013 reported 66.5% of women with syphilis suffered avoidable adverse pregnancy outcomes from stillbirth to neonatal complications.3,6
Comparatively, congenital syphilis is uncommon in the UK. Screening coverage in pregnancy is 99% and the UK has achieved the 2007 WHO target of 50 or fewer cases per 100,000 live births and thus ‘elimination of mother-to-child transmission of syphilis’. Only 21 diagnoses of congenital syphilis occurred in England between 2010 and 2017. Of these, nine women had antenatal screening records and seven had a negative first trimester antenatal screen, suggesting infection occurred later in pregnancy.1
Worryingly, in recent years Public Health England (PHE) data have reported rising rates of syphilis cases in the adult population with an increase of 162% between 2008 and 2018, and a further rise by 10% in syphilis cases from 2018 to 2019.7 We can infer from this that we may see a rise in the diagnoses of congenital syphilis in the coming years. There has also been a documented rise in atypical cases of congenital syphilis in neonates born to mothers with negative first trimester screening, as was the case with our patient.8 To address this rise in syphilis cases, PHE has launched an action plan which includes maintaining high antenatal screening coverage and vigilance for syphilis throughout antenatal care. Further syphilis testing in the later stages of pregnancy should be offered to women whose apparent risk of acquiring a sexually transmitted infection (STI) has changed during the pregnancy. Examples of such changes include, injecting drug use, sex work, a partner with a diagnosed STI or a known male bisexual partner.1 This of course does not cover every case. We believe that in this case study, infection of Baby S occurred later in pregnancy as blood tests at booking had a negative VDRL screen. This mother would most likely have benefited from the later screening, although would not have been classified as ‘high risk’. Sexual health histories should be taken routinely throughout pregnancy to identify any changes to the mother’s lifestyle and high-light new risks for infection.
The clinical manifestations of syphilis, the great imitator, have been described for centuries. Even in the newborn period, syphilis can imitate other neonatal infections and a high index of suspicion is required to make a timely diagnosis and institute appropriate treatment.
Clinical manifestations of live births are extensive, variable and a direct result of the inflammatory response that occurs when T. pallidum is disseminated throughout the fetal organs. Common clinical signs include:10
- low birth weight
- hepatosplenomegaly
- severe jaundice
- anaemia
- skin rash (almost any form)
- ulceration of the nasal mucosa
- failure to move an extremity (pseudoparalysis of Parrot)
- condylomata lata
- rhinitis (may be a late sign).
The bones, liver, pancreas, intestine, kidney and spleen are the most frequently involved but the severity of clinical presentation is unpredictable.9 Presentation can be vague and if syphilis status is unknown or assumed to be negative, symptoms and signs could easily be attributed to other illnesses.
Approximately two-thirds of infants with congenital syphilis are asymptomatic at birth, although most will present within the first five weeks.11 Hepatomegaly is seen in almost all infants with congenital syphilis.12 40-60% of other babies will have at least one other common feature including jaundice, anaemia, splenomegaly with hepatomegaly, lymphadenopathy, non-immune hydrops, low birth weight, prematurity and pyrexia. Skin rash of any kind can be seen – maculopapular, vesicles or bullae or even condylomata lata (flat wart-like plaques on the genitals).12 Ulceration of the nasal mucosa can occur and rhinitis may present in the first week. More pathognomonic symptoms include failure to move an extremity due to pseudo-paralysis (pseudo-paralysis of Parrot), osteochondritis or periostitis.12
All at-risk infants should have syphilis serology performed for T. pallidum syphilis IgM, although it should be noted a negative IgM does not exclude syphilis.12-14, These should be accompanied by a maternal venous blood sample for comparison of non-treponemal tests (ie VDRL carbon antigen test or RPR). These are indirect biomarkers of cell damage by the syphilis spirochete.14 If the infant VDRL or RPR titre is 4x greater than the maternal sample, this is indicative of congenital syphilis.14 Paired TPPA testing can also be sent for. Additionally, dark-field microscopy and PCR testing can be performed on body fluids (rhinitis) or from lesions, eg a bullous rash (TABLE 3).13-15
Where there is suspicion of congenital syphilis, infants should also have investigations for: full blood count, white cell count, urea and electrolytes, liver function tests, HIV antibody, lumbar puncture for CSF, protein, RPR and TPPA. Long bone X-rays can be taken for osteo-chondritis and periostitis, a chest X-ray for cardiomegaly, a cranial ultrasound scan, an ophthalmology assessment for interstitial keratitis and audiology for eighth nerve deafness (TABLE 3).13
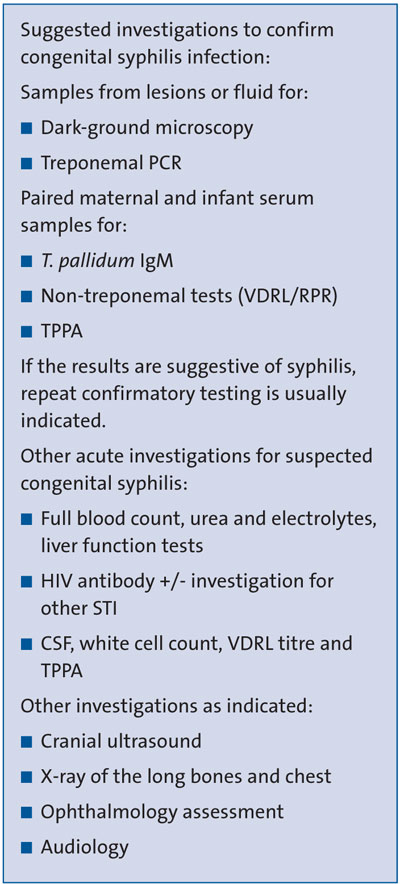
TABLE 3 Suggested investigations where there is suspicion of congenital syphilis.11,14
Penicillin is the treatment of choice for congenital syphilis and our patient received a 10-day course of intravenous penicillin. It is also the treatment of choice for adults with syphilis.
Conclusion
As syphilis is a great imitator and infection rates are on the rise, neonatologists and paediatricians should have a high index of suspicion for congenital syphilis infection in the unwell neonate, irrespective of negative blood tests at booking, as maternal serology may have changed during the pregnancy. Prompt diagnosis of congenital syphilis is imperative as early diagnosis and treatment can prevent long-term morbidity and mortality.
Patient consent, acknowledgment and author contributions
Consent was obtained from the patient’s mother. Dr Lakshmi Chilukuri, Paediatric Consultant, Whiston Hospital, was the named consultant for the child. Dr Ijaz Ahmad, Paediatric Consultant, Whiston Hospital, was the on-call consultant who led the management of the patient prior to transfer to the tertiary unit. Dr Tochi Igboekw had the idea for the report, gained consent from the mother and contributed to the writing of the discussion and conclusion. Dr Khalida Yasso wrote the title page, scope, keypoints and keywords, background section, case section, and edited the format, layout and references. Dr Emily Thomas contributed to the writing of the discussion and conclusion and edited the report. Dr Emily Rye contributed to the writing of the case section. Dr Sally Ogden contributed to the writing of the case section.
Or read this article in our
Tablet/iPad edition
- A recent report found that rates of congenital syphilis are on the rise for the first time since 2013.
- Congenital syphilis infection in the unwell neonate should be suspected despite negative antenatal blood tests, as maternal serology can change during pregnancy.
- Prompt diagnosis of congenital syphilis is imperative to prevent long-term morbidity and mortality.
Also published in Infant: