Perinatal post-mortem consent: a national survey
This project examined the experiences of healthcare professionals who obtain consent for perinatal post-mortem examination with the aim of using the findings to develop training resources for taking post-mortem consent.
Hannah Wood1
Consultant Neonatologist
h.wood5@nhs.net
Joanne Cookson2,3
Practice Educator WMNODN / Neonatal Lecturer Keele University
j.cookson@keele.ac.uk
Asha Shenvi2,4
Consultant Neonatologist UHNM / Medical Education Lead WMNODN
asha.shenvi@uhnm.nhs.uk
1NICU, Birmingham Women’s and Children’s NHS Foundation Trust
2West Midlands Neonatal Operational Delivery Network (WMNODN)
3School of Nursing and Midwifery, Keele University
4NICU, Royal Stoke University Hospital, University Hospitals of North Midlands (UHNM) NHS Trust
Following a stillbirth or neonatal death there is an opportunity to perform a post-mortem examination. It is recommended that unless the death is being referred to the coroner, all parents whose baby has died should be offered the opportunity to discuss having a post-mortem so that they can make an informed choice.1,2 A post-mortem may confirm a diagnosis, provide new information that changes a diagnosis or provide some additional information.3 It is therefore a valuable investigation following a stillbirth or neonatal death.
The Mother and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK (MBRRACE-UK) reported 2,579 stillbirths and 1,199 neonatal deaths in 2018.4 While a post-mortem was offered in 97.1% of stillbirths and 84.6% of neonatal deaths, consent for a full or limited post-mortem was given by half of the parents of stillborn babies and just over a third of the parents of neonates who died.4 This reflects a small increase in the rate of consent for post-mortem following stillbirth and neonatal death since 20162 but overall, post-mortem consent rates remain low. Furthermore, it has been reported that parents who declined a post-mortem examination were approximately twice as likely to regret their decision compared with those who consented.5
Obtaining consent for post-mortem differs from other procedures as consent is usually sought by health professionals who do not perform the procedure. Professionals therefore need a good level of knowledge and understanding of the procedure to be able to support parents to make a decision.6 Offering and obtaining consent from parents after the death of their child is challenging and healthcare professionals do find this difficult.6,7 Multiple barriers to consent have been identified. A lack of specialist training and ensuing inadequacy in knowledge, confidence and experience has been reported by professionals and parents.6,8 Addressing these barriers may help to improve uptake rates.
In 2013, Sands (the stillbirth and neonatal death charity) announced learning outcomes to help improve and standardise training for consent takers. Until then, there were no agreed training standards for seeking post-mortem consent and the provision of training on consent taking was inconsistent.1 As recommended by Sands and also advocated by the Human Tissue Authority, all consent takers should be trained and specifically approved to take consent for a post-mortem, and should have observed a post-mortem examination, ideally that of a baby.1
We aimed to explore the current experiences of health professionals who are likely to take consent for post-mortem examination. We specifically focused on their training experiences and intended to use this information to guide the development of a new training resource.
Method
A national online survey of UK healthcare professionals’ experiences of obtaining consent for post-mortem examination was performed between May and October 2018. The questionnaire was designed by a working group that included a neonatologist, obstetrician, practice educator, bereavement midwife and a neonatal sub-specialty trainee. It aimed to seek health professionals’:
- opinions of post-mortem
- knowledge of post-mortem
- experiences of obtaining consent for post-mortem
- training on the consent process.
Health professionals who were expected to obtain consent for post-mortem were invited to participate and included professionals from paediatric, neonatal, obstetric, midwifery and bereavement backgrounds. The web link to the survey was shared using multiple forums:
- the national operational delivery network administrators distributed the weblink to professionals practising within their network
- the national obstetric and neonatal specialty training representatives distributed the weblink to the obstetric and neonatal trainees
- the West Midlands paediatric deanery administrator distributed the weblink to the regional paediatric trainees. The survey was also advertised on their trainee-led social media page
- the survey was highlighted to attendees during a West Midlands pathology study day
- the weblink was also made available on the consultation page of the British Association of Perinatal Medicine (BAPM) website.
Results
There were a total of 122 responses. This included 80 (66%) paediatric and neonatal staff, 33 (27%) obstetric and midwifery staff and 9 (7%) from bereavement teams (TABLE 1). Paediatric and neonatal profes-sionals responded from across the national neonatal operational delivery networks, whereas obstetric, midwifery and bereave-ment professionals responded largely from the West Midlands (57%). The majority of respondents were doctors (83%).
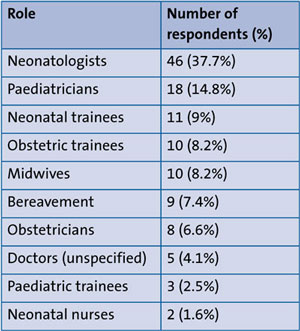
TABLE 1 The roles of health professionals responding to the survey (n=122).
Opinions, knowledge and experiences of obtaining consent for post-mortem
The majority of respondents obtain consent for post-mortem (80%) on a regular (29%) or occasional (51%) basis. There were respondents who never take consent (20%). This was not limited to a particular professional group and included: six neonatal sub-specialty trainees, five midwives, three neonatologists, three specialty doctors, two paediatricians, two paediatric trainees, two obstetric trainees and one neonatal nurse. Although these professionals do not currently obtain consent, some of these groups will need to achieve competence in this skill during training as they may become consent takers in future. Furthermore, all have a role in supporting parents through this experience and therefore should be aware of the process. For these reasons we chose to include this group in the analysis.
The majority of respondents agreed that all parents should be offered a post-mortem examination following a stillbirth or neonatal death (94%). Over half (54%) responded that a post-mortem changes the diagnosis in 10-30% of cases. However, 17% responded that it changes the diagnosis in <10% and therefore underestimated the value of post-mortem.
Respondents were asked to list the information they would discuss with parents when obtaining consent for post-mortem. Responses were compared to the themes advised by Sands within their ‘Guide for consent takers’3 and are listed in TABLE 2 in order of most frequently reported issues for discussion.
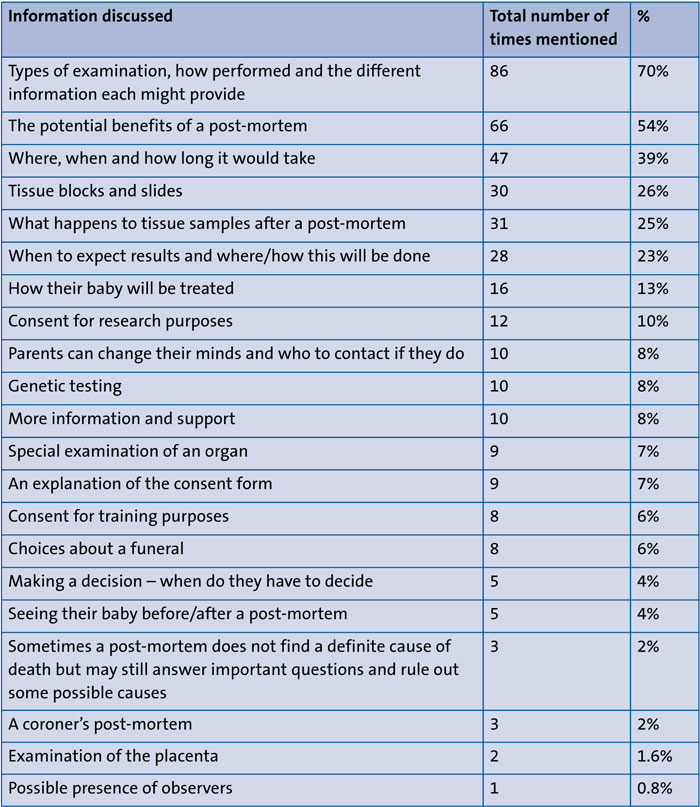
TABLE 2 Information respondents would discuss when obtaining consent for perinatal post-mortem. Note that respondents were able to provide multiple responses to this question.
Written information is offered by 79% of respondents including (from most to least commonly reported): local information, information leaflet (unspecified), information from a charity (eg Sands), copy of consent form, information from the region or network, information from the pathology department or national information.
Training on the consent process
Just over half of the respondents are trained to obtain consent for post-mortem (57%). Of the 43% who are untrained, 58% obtain consent in clinical practice and do so regularly (13%) or occasionally (44%). This is not limited to a particular health professional group (TABLE 3).
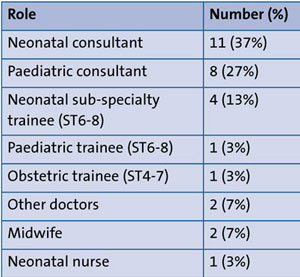
TABLE 3 Consent takers without training (n=30).
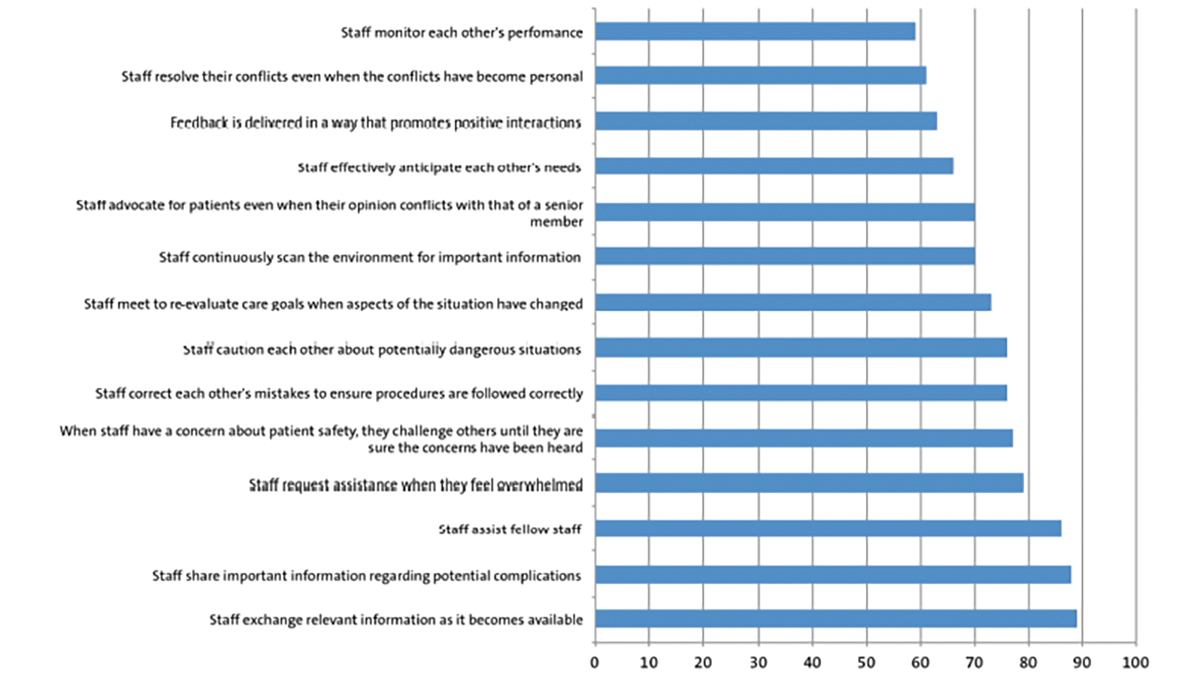
Those who are trained listed 18 different types of training (FIGURE 1). Teaching from colleagues followed by attending a dedicated study day, and observing a post-mortem were the most commonly reported training methods. Interestingly, 51% of total respondents and 41% of consent takers have not observed a post-mortem. Just under half of respondents were not aware of information resources that may help them prepare for seeking consent (49%). Those aware of resources, most commonly reported the information from Sands. Respondents referred to other resources such as a local guideline (n=8), consent form (n=5), the Human Tissue Act (n=2) and patient information leaflet (n=1).
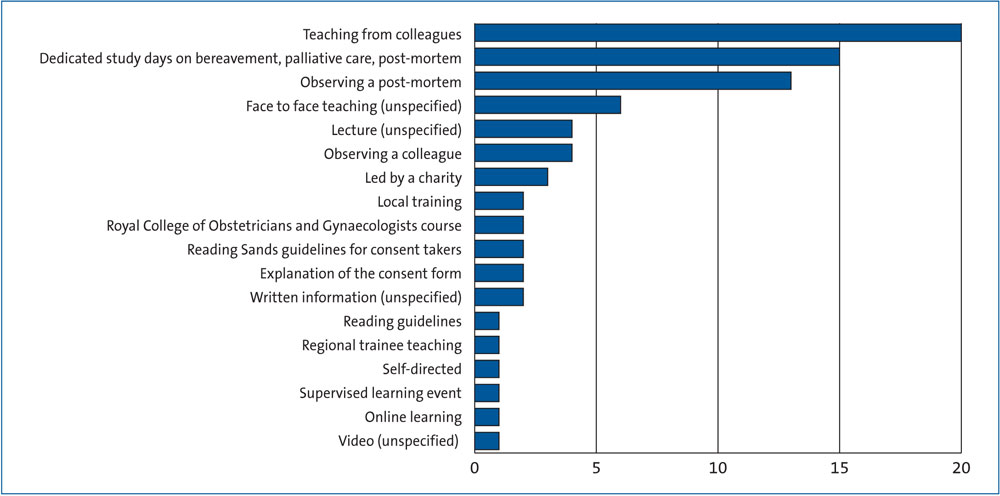
FIGURE 1 Types of training reported by respondents. Note that respondents were able to provide multiple responses to this question.
Confidence levels were variable with 14% who felt ‘extremely confident’, 31% ‘very confident’, 26% ‘somewhat confident’, 17% ‘not so confident’, and 12% ‘not at all confident’. The majority, therefore, felt confident to obtain consent (71%). Of those who felt ‘not so confident’ or ‘not at all confident’, 62% never obtain consent. However, 13% of those who take consent admitted lacking confidence. This group included one neonatologist, three paediatricians, two neonatal sub-specialty trainees, one senior paediatric trainee, one obstetric trainee, one ex-trainee, one neonatal nurse, two midwives, and one member of the bereavement team.
When asked if more extensive and accessible training is needed, 82% agreed. For one respondent, the survey highlighted this as an outstanding educational need to be achieved prior to completing specialty training. Respondents commented on what the training should consist of. It should be ‘standardised’, ‘accessible’, ‘free’ and endorsed by the professional bodies. A variety of training methods were suggested including online learning, observing a post-mortem, simulation, study days and supervised learning events. It should incorporate videos, animation and photos to illustrate the process of a post-mortem. The expertise of a pathologist should be sought when designing the content. Respondents requested specific training on the information that should be discussed with parents, the consent form, communication skills, religious and cultural considerations, how to respond to commonly asked questions by parents, and available links to further guidance. They also felt there should be resources for parents to use. Respondents recommended that it should be included within core obstetric, paediatric and midwifery training. They echoed the advice from Sands that health professionals should be signed off as competent before obtaining consent in clinical practice. An option for refresher training was requested as a method of maintaining competence.
Discussion
This survey has identified that the Sands’ prerequisites for consent takers are not being met (TABLE 4).3
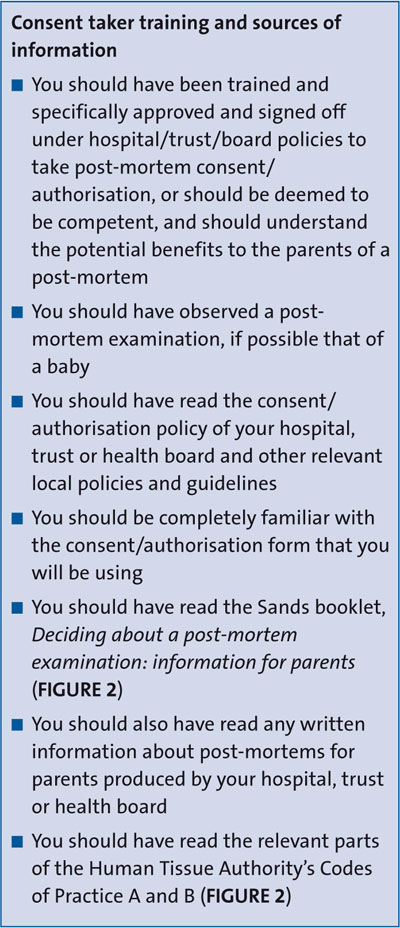
TABLE 4 Prerequisites for consent takers (Sands).3
The majority of respondents were existing consent takers and most had some form of training. This is an improvement from a national survey of neonatal consultants that found that 80% received no formal training in obtaining consent for post-mortem.7 However, there continues to be a group who are not trained. This includes existing consent takers, those who do not currently take consent but who may do in future, and those who never take consent. Irrespective of this, almost all respondents will have a role in supporting parents through a bereavement. Therefore, professionals still need a level of understanding about post-mortem in order to care for the family following a stillbirth or neonatal death. Professionals who do not currently take consent but who may do in the future, includes trainees who will need to demonstrate competence prior to completing specialty training. When the survey was undertaken, the neonatal medicine sub-specialty curriculum stated that trainees be competent to ‘counsel and obtain consent for neonatal post-mortem examination’. Our survey therefore suggests that for some trainees, this may not be achieved during their training and they may encounter this for the first time as consultants.
Almost all respondents felt parents should be offered a post-mortem following a stillbirth or neonatal death. This attitude among professionals is reassuring as a first step towards increasing post-mortem uptake rates. It is also higher than previously reported where only 60% of consultant neonatologists would routinely offer a post-mortem examination.3
Evidence suggests that a post-mortem can change the diagnosis or additional findings in 22-76% of cases.9 In a study of post-mortem examinations for premature infants of <28 weeks’ gestation, there was a significant change in diagnosis in 28% of cases.10 According to Sands, between 10-30% of post-mortem examinations provide new information that changes the diagnosis. In our survey, over half (54%) correctly identified the proportion in which a post-mortem changes a diagnosis, however, there was a group of respondents who underestimated the value of a post-mortem. More education is therefore needed to improve consent takers’ understanding of the potential benefits of post-mortem.
Respondents who are trained reported multiple methods of training with ‘teaching from colleagues’ being the most common. The variety of training methods reported by respondents and the likelihood that training from colleagues is highly variable, indicates that provision of training remains non-standardised. Available training can also be limited by regional resources as illustrated in our region where pathology training days are too infrequent to meet the demand. It has been previously reported that even when professionals are trained, they can feel dissatisfied with the training received.9 Despite being the third most commonly reported form of training, most respondents have not observed a post-mortem. In addition to being a Sands’ prerequisite, witnessing a post-mortem is associated with improved knowledge of the procedure, greater confidence in consenting and better satisfaction of training among professionals.5,10
Sands states that consent takers should have read their information booklet for parents in addition to any written infor-mation produced locally. The majority of respondents offer written information to parents and both of the aforementioned were commonly offered resources.
The prerequisites also recommend being familiar with a number of additional resources including the local policy/guideline, consent form, and the Human Tissue Authority’s Codes of Practice A and B. Just over half of respondents were aware of resources that may aid their preparation but the aforementioned resources stipulated by Sands were very infrequently reported.
Professional advice influences parents’ decision to consent for post-mortem.4,5 Confidence levels will affect the information given and the manner in which it is delivered by professionals. Although overall confidence levels among respondents were variable, most reported a degree of confidence to obtain consent. This is not reflected by the high propor-tion of respondents who felt that more training is needed in this area. This does, however, echo the results of previous studies in identifying the need for further education and that consent takers would support this.6,8
Conclusion
This national survey identified that the Sands prerequisites for consent takers are not being met and highlights the need for standardised training. There appears to be consensus among health professionals that all parents should be offered a post-mortem examination following a stillbirth or neonatal death but despite this, uptake rates remain low. This national survey identified that a significant proportion of health professionals involved in providing bereavement care are not trained on perinatal post-mortem. Even when health professionals are trained, the training is variable between individuals. As an expected consequence, some health professionals lack confidence about discussing post-mortem with parents and the conversations held are unlikely to be consistent.
In order to address this gap in training, the University Hospitals of North Midlands in partnership with Keele University and the West Midlands Neonatal Operational Delivery Network (WMNODN) have developed a new e-learning resource. This is mapped against the learning outcomes stipulated by the Human Tissue Authority and Sands, and encompasses many of the suggestions from the survey respondents. This standardised online resource is hosted by Healthcare Education England e-Learning for Healthcare and was launched in 2020 (www.e-lfh.org.uk/programmes/perinatal-post-mortem-consent).11 We anticipate this will improve the knowledge and confidence of health professionals seeking consent from bereaved parents for post-mortem and subsequently impact uptake rates positively.
Or read this article in our
Tablet/iPad edition
- National recommendations state that all consent takers should be trained and specifically approved to take consent for a post-mortem examination. A lack of specialist training is a barrier to consent.
- Our survey found that the Sands pre-requisites for training consent takers are not being met. Consent takers desire standardised, accessible and free training. Encompassing the findings, an interactive e-learning resource has been developed to meet the consent takers’ needs.
Also published in Infant: